Chapter Four
ASC Revenue Cycle Challenges and Opportunities for Improvement

"Cash flow is king" for businesses, and it's no different when it comes to maintaining a successful ASC operation. Implementing a streamlined workflow and leveraging the latest technologies can help you shorten the revenue cycle to get paid faster and collect a higher percentage of outstanding payments from patients.
Consider the following key strategies to help you overcome revenue cycle challenges and uncover opportunities for improvement:
Examine Your Revenue Cycle
Here are three areas of focus that can help you shorten your billing cycle to improve cash flow and the financial health of your ASC.
1. Enhance billing performance
Effective and efficient ASC billing is contingent upon numerous factors. Billing staff must be skilled in their craft and receive ongoing education to keep current with changing rules. Physicians must provide the right information so billers and coders can perform their duties. IT systems must be configured to support an ASC's specific needs and requirements.
Follow these 10 steps to boost your billing performance:
- Collect relevant and accurate financial data (e.g., payer mix, service mix, physician productivity, implant usage) to identify issues that can negatively impact revenue cycle performance.
- Analyze the financial performance data, generate reports, and extract insights to drive strong decision-making.
- Benchmark performance data annually to enhance ASC billing and overall revenue cycle performance.
- Set reasonable billing goals and identify barriers to help you focus your resources on making targeted improvements.
- Provide the training and education your staff needs to overcome obstacles and drive progress toward your goals.
- Monitor ongoing results and share feedback with employees to ensure that you are on track to meeting your objectives.
- Hold staff accountable for their results to encourage team members to come up with solutions proactively.
- Audit performance data and review the results to see if your strategy is working.
- Communicate frequently with your staff about their performance and bring the team together to discuss progress.
- Repeat the process quarterly: Analyze your revenue cycle, look at your data, set new goals, and implement workflows to achieve them.
2. Improve the patient payment collection process
With patients increasingly responsible for a greater portion of their healthcare costs, ASCs must effectively collect these higher amounts while considering the potential stress and distress patients may experience under the financial pressure.
Here are 10 steps to help you collect payments more effectively without hurting — and possibly improving — patient satisfaction:
- Educate all staff members, including physicians and the staff of affiliated practices, about the importance of point-of-service collections.
- Establish a standard collection process and make sure it's followed consistently. Once those guidelines are implemented, staff should never deviate from them.
- Improve your collection process by analyzing data, identifying opportunities, and making incremental adjustments.
- Ask the staff involved in the collection process for ongoing suggestions. Provide the resources they need to help them perform more effectively.
- Learn from challenging experiences to see how you can prevent the incident from happening again or turn a negative experience into positive changes.
- Train your staff to approach every patient interaction with empathy and respond appropriately to the reactions they may face when discussing a bill.
- Show your staff how to identify patient warning signs so they can effectively defuse a stressful situation and improve collections.
- Make sure that discussions about point-of-service collections are conducted in private. Develop processes to collect from patients before the day of surgery to minimize these conversations and their potential impact on patients and their stress on the day of surgery.
- Establish a clear policy and communicate to patients which payment method you accept to minimize unpleasant surprises for the patients.
- Set your goal to 100% collection to encourage your staff to aim high and strive for top performance.
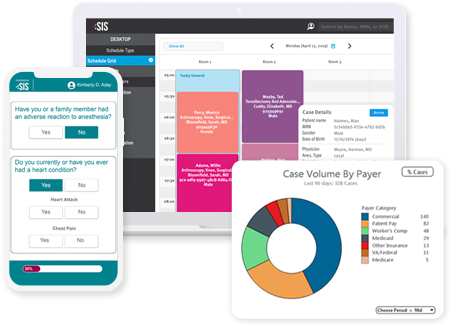
3. Leverage technology to improve the revenue cycle
Technology can enhance an ASC's billing and collection efforts. It can improve claims completion and submission speed, boost staff productivity, decrease payment time, and reduce expenses. ASCs that understand how to maximize their investment in a software solution will reap the most benefits.
Here are 10 tips to effectively leverage ASC software and technology to improve your revenue cycle:
- Take the time to research and assess the system(s) you are considering.
- Focus initially on building comfort and confidence in using a platform's core functions.
- Explore, learn, and use the advanced features once you are comfortable with the basics.
- Assess new features and determine if they are helpful to your ASC.
- Offer the assistance and resources your staff needs to use the new technology efficiently.
- Use competency testing to ensure employees are using the software productively.
- Make it clear that everyone will be using the solution — no ifs, ands, or buts.
- Inform physicians about their responsibilities concerning usage of the new technology.
- Monitor staff productivity and satisfaction so you can respond quickly to potential issues.
- Include software and technology as a topic in your patient surveys to ensure that it is making a positive impact on the patient experience.
Improve ASC Coding Accuracy
The consequences of poor coding in an ASC can be severe. Inaccurate coding can lead to lost revenue, unnecessary expenses, insurance audits, angry patients, and even trigger fraud investigations. Limiting the number of coding errors and quickly addressing those that occur are critical to a high-performing, compliant revenue cycle.
Support coders by keeping them informed about all the changes in your ASC that can impact their work. This includes developments concerning payers, procedures, physicians, specialties, and surgical technology. Show physicians how they can help improve the coding process by completing detailed operative reports, staying current on documentation changes, and demonstrating a willingness to speak with coders to resolve questions promptly.
Hire coders with ASC-specific coding experience and provide them with ongoing education and training. This helps ensure that they stay current with the latest coding rule changes and best practices to minimize errors and delays.
Whenever your ASC experiences a denial, review it carefully to determine the cause. If the rejection is associated with a coding error, educate coding staff on how to avoid the mistake from occurring again. Also, conduct routine audits to detect errors missed by payers. If an audit identifies mistakes, provide relevant education to coders.
Set quality- and quantity-based performance goals for your coding staff and motivate them with rewards to improve performance. Additionally, develop a plan to handle coder absences and manage workload with better coder scheduling during busier or growth periods.
Undergo annual, third-party assessments to stay current with the latest best practices and identify areas for improvement. Lastly, consider outsourcing your coding and billing functions to a reputable provider to help increase clean claims percentage, better ensure timely and accurate collections, and reduce denials and payment delays.
Understand Reimbursement Trends
Changes concerning reimbursement can have a significant impact on how an ASC performs collections and negotiates its managed care contracts. Here are six significant ASC reimbursement trends and developments from the past few years that you should be aware of.
1. Alignment of payment update factors
CMS's 2019 final payment rule aligned ASC and hospital outpatient department (HOPD) payment update factors from 2019 through 2023. This means ASC payment rates would be updated using the hospital market basket inflation factor instead of the Consumer Price Index for All Urban Consumers (CPI-U).
ASCs should see an increase in their CMS reimbursement through 2023 compared to what they would have received had CMS not aligned the payment update factors. Since commercial payers often base their reimbursement rates on a percentage of Medicare, ASC may see an increase in commercial reimbursement.
2. Coverage of more complex ASC procedures
CMS has been gradually adding spine, cardiovascular, total joint, and other complex procedures to the ASC-payable list. It has also been removing many codes from the inpatient-only list so they can now be performed in the hospital outpatient setting. This is often the first step in such procedures eventually being added to the ASC list. In the 2021 Medicare hospital outpatient prospective payment system and ambulatory surgical center payment system final rule, CMS finalized its proposal to eliminate the inpatient-only list over a three-year transitional period, beginning with the removal of approximately 300 primarily musculoskeletal-related services, with the list completely phased out by CY 2024.
While many private payers have covered more complex procedures in ASCs for years, the decision by CMS to add them to the payable list allows ASCs to perform the surgeries on Medicare beneficiaries and receive reimbursement for the services. Private payers on the fence about whether to provide their own coverage may be swayed by CMS's decision to do so.
3. Shift toward value-based payments
While fee-for-service remains the dominant payment model for ASCs, there is a gradual shift toward value-based payment models, mostly in the form of bundled payments. Bundled payment arrangements are designed to pay multiple providers for coordinating the total amount of services required for a single, predefined episode of care. Providers can share in the savings if they keep costs below the target price while maintaining quality standards.
Total joint replacement is a good example that can benefit from this format. Such a bundled payment could cover the surgical fee, ASC fee, implants, anesthesia, physical therapy, and medications.
4. Increased patient financial responsibility
When patient responsibility for their surgical care was low, ASCs could typically remain profitable if they focused on collecting reimbursement from payers. This has changed in recent years, with patients now responsible for a much larger portion of their healthcare costs. As such, ASCs need to give attention to both payer and patient payments by implementing an effective collection process that ensures on-time payment while considering the emotional or financial challenges that patients may face.
5. Bypassing ASC reimbursement
Some ASCs are offering patients a self-pay option for their surgical care in which patients are responsible for covering all the costs associated with their procedure(s). In this model, ASCs do not bill or collect reimbursement from payers. Such an approach is particularly beneficial if ASCs are interested in attracting medical tourism (i.e., performing procedures on patients outside of their market/coverage area).
While some ASCs rely exclusively on the self-pay model, others are embracing a blend of self-pay and covered procedures to grow volume and cater to patients who may want to avoid using their insurance for coverage of their surgical care.
Recognize the Importance of Clean Claims
A clean claim rarely gets rejected or denied. Assuming a payer abides by its contract, a clean claim does not need to be filed more than once because of errors. It goes out your door, requires no additional work, and is paid. Almost all ASC key performance indicators (KPIs) are impacted by how fast the center can get claims out the door and how frequently claims are denied or rejected.
Clean claims also help ASCs increase staff productivity because you may be able to reassign staff to other tasks or even reduce staff when your denial and rejection late is low. You will save on the expenses associated with re-working claims and submitting. Having a high clean claim rate can help you hit all your ASC's financial objectives and be in a better position to stay on budget.
Here is how you can improve your ASC's ability to submit clean claims:
First, everyone involved with getting a clean claim out the door in a timely manner — from physicians to coders and billers — must understand the pivotal roles they play and how shortcomings can have significant short- and long-term effects on an ASC's financial viability. Then, set goals to target a 100% clean claim rate to encourage everyone to scrutinize denials, rejections, and delays, then implement fixes to reduce the likelihood of them occurring again.
Detail all the steps that employees must take to better ensure the complete, accurate completion of claims. Help your staff follow these processes by providing cheat sheets and other resources. New staff members should be able to understand the steps and their responsibilities quickly and easily. Furthermore, address what employees should do if they have a question or concern about a claim. They should feel confident that every claim going out the door is as complete and clean as possible.
Be prepared to review and update your workflows to increase staff efficiency. Hold staff accountable for following your processes and achieving objectives. Also, help your employees succeed by providing ongoing support. For example, send team members to state or national meetings; allocate funding for certifications, online courses, and webinars; and purchase books, manuals, and cheat sheets.
Use the right technologies and maximize your investment in them by learning the ins and outs of your solutions. Take the time to discover new features or older functions you have not been using that can make claims processing more effective and efficient. Ask your ASC software and technology vendors for guidance. You may be surprised to learn what handy tools are at — or will soon be at — your fingertips.
Regularly assess your performance and processes to discover areas for improvement. If your clean claim rate starts to decline, do not wait to respond. Dive into your data right away and identify the cause(s) so you can implement fixes as soon as possible.
Finally, getting out clean claims is all about teamwork. ASCs with the highest clean claim rate tend to have staff who work well together and communicate effectively. When employees not only work hard but also support one another, an ASC's performance improves. But when communication is poor and departments operate as silos, with staff members only concerned about their own work, this will drag down revenue cycle performance and KPIs.
Achieve Managed Care Contracting Success
Strong managed care contracting improves the financial health of an ASC. Proper preparation is key to achieving success in this area. Gather internal and external data to help you understand your ASC's direct and indirect costs, your competitive advantage among other ASCs, your market's payers and their plan types, state fees, Medicare rates, CMS fee schedules, and other information applicable to managed care contracting. Review all the information and research the payers you are looking to target.
Then, organize your research to support negotiations with payers. If you understand their market, reimbursement methodology, and types of contracts and understand what you need to remain financially viable and profitable before you begin the negotiations, you have a better chance at getting the terms you want.
Establish your timelines and set reasonable goals to help you stay on track and meet contracting deadlines. When you enter a negotiation with a payer, be confident. During the research and organization step, you should have calculated bottom-line numbers that you are willing to agree to in the managed care contract. Always be reasonable — payers will be more likely to work with you if you negotiate in good faith and do not make outrageous requests.
Work to a build relationship with someone in the payer's team and foster a mutually beneficial relationship. Keep the payer's business model front and center during the negotiation so they are more likely to treat you as a partner, not a competitor. Also, be willing to "give some to take some" during negotiations to build an ongoing relationship that will benefit your ASC in the long term.
Once you have the contract signed, the work is not over. Set expectations from the start to check in frequently with the payer to measure progress and discuss misinterpretations either party may have run into post-agreement. Include payer contracting as part of your routine and revisit those contracts periodically to ensure that they reflect the latest changes in your facility and regulations.
Back to Top
 The Nuts & Bolts of a Successful ASC Self-Pay Program
The Nuts & Bolts of a Successful ASC Self-Pay Program